Initial Referral to Oncology
Sophie is a 7-year-old female spayed Golden Dachshund who was first presented to her primary veterinarian for a routine health check. Routine bloodwork revealed markedly elevated liver enzyme levels and moderate anaemia. Further investigation with an abdominal ultrasound revealed a liver mass, with a suspicion for malignancy and a poor prognosis – this prompted referral to our oncologist, Dr Danielle Gibson, for assessment and treatment planning.
On presentation to Dr Danielle, Sophie was clinically well, with no significant abnormalities noted on physical examination. Sophie was then admitted for a further abdominal ultrasound, performed by our radiologist Dr Jose Labrador. Based on the imaging findings, a large mass associated with the liver was confirmed, with Dr Danielle’s top suspicion being hepatocellular carcinoma.
Learning Point #1
In liver masses in dogs, it is easy to assume that a large mass = a bad mass. However, masses such as haemangiosarcomas often rupture before they ever get to a significant size.
The top differential for a large liver mass is usually a hepatocellular carcinoma, which has a much better prognosis compared to haemangiosarcomas.
Transfer to Surgery
In this case, Dr Danielle advised that surgery was the preferred treatment option for a suspected hepatocellular carcinoma.
Sophie was then transferred to our specialist surgeon, Dr Naomi Shimizu, who recommended a preoperative CT scan to assess resectability and vascular involvement.
CT Imaging
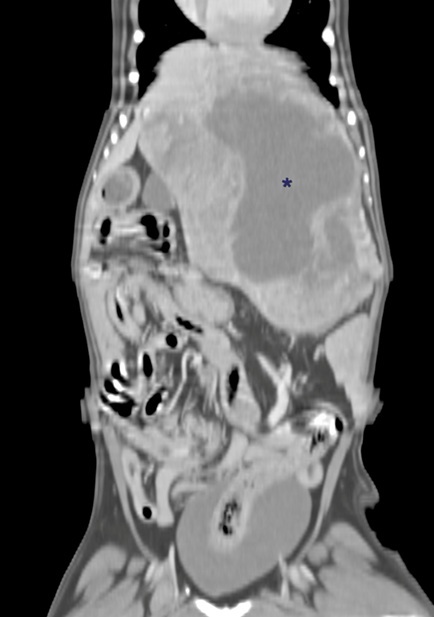
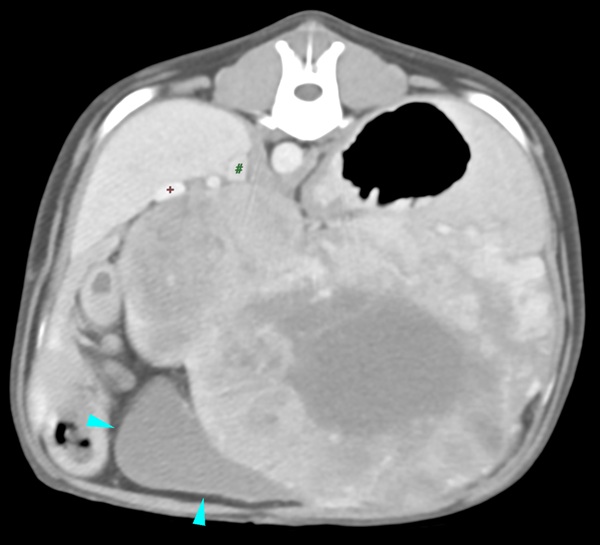
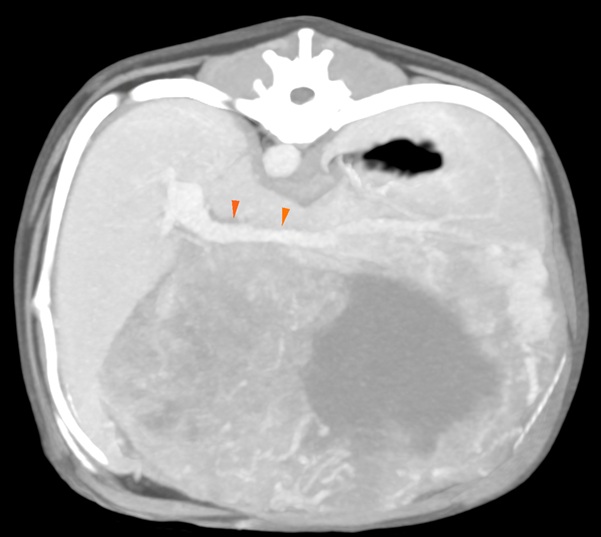
Sophie was admitted at a later date for her CT scan and potential surgery. The CT scan findings were as follows:
- A large (~15cm x 12cm x 8cm) well-defined hepatic mass arising from the quadrate lobe
- Marked mass effect and vascular displacement, particularly involving the caudal vena cava and portal vein
- No evidence of metastasis on thoracic CT
The following images show the visualisation of the mass on CT, as well as how the surrounding structures are impacted by the mass:

Surgical Intervention
Despite the risk of significant haemorrhage and incomplete margins, surgery was recommended due to the likelihood of eventual rupture and haemoabdomen if the mass was left unchecked.
Under Dr Naomi’s charge, a challenging but successful liver lobectomy was performed. Due to the extent of the tumour, cholecystectomy was required to facilitate excision. As our team had predicted, intraoperative haemorrhage was encountered, necessitating a blood transfusion. However, the team was well prepared for this outcome – as blood donors had been secured prior to the procedure, the blood transfusion was effectively managed by our general anaesthesia team and anaesthesia specialists, and Sophie remained stable throughout the procedure. She was monitored postoperatively in our ICU, where she received intensive supportive care.
By the next morning, Sophie was bright, alert, eating, and stable. She was discharged two days post-op with pain management and strict rest instructions.
Multidisciplinary Approach Enhances Treatment Success: The seamless collaboration between our oncology, surgery, radiology and anaesthesia teams ensured optimal case management, from initial diagnostics to surgical resection and eventual discharge. Our integrated approach can maximise survival outcomes and quality of life for pets.
Final Diagnosis & Prognosis
A week after surgery, histopathology results confirmed that Sophie did indeed have moderately differentiated massive hepatocellular carcinoma (HCC). This is the most common primary liver tumour in dogs, and outcomes following surgical excision are generally favourable.
While margins were incomplete, this is not typically prognostically significant, as recurrence is rare and slow-growing. Median survival time is approximately 900 days, with some dogs surpassing this significantly. No further treatment was required for Sophie, and she remains happy and healthy today!
Learning Point #2:
Early Oncology Referral Can Improve Outcomes: What was initially assumed to be a high-risk case with a potentially poor prognosis turned out to have an excellent prognosis with surgical intervention. Oncology evaluation can provide vital diagnostic clarity and guide appropriate treatment.
Conclusion
This case highlights the importance of early oncology intervention and the benefits of a coordinated, multidisciplinary approach in complex oncology cases. With the combined expertise of Dr Danielle and our surgical specialist team with Dr Naomi, Dr Daniele and Dr Jayson, VES provides Singapore’s leading surgical oncology service for referring veterinarians and their patients.
If you have questions about any case at all, we highly encourage you to contact us to speak with our oncologist or surgeons at 6266 0232 – we are always available and happy to help you out!